Guides
What is IUI? The Process, Success Rates, & Cost of Intrauterine Insemination
The IUI process
If you’re going in to see a fertility specialist for the first time to help you get pregnant and they recommend you to do treatment, their first suggestion may be to try an IUI cycle.
IUI stands for intrauterine insemination, also known as artificial insemination (AI).
Intrauterine insemination is often the first line of treatment that a reproductive endocrinologist would suggest for couples who have been having difficulty getting pregnant.
Intrauterine insemination is often the first line of treatment that a reproductive endocrinologist would suggest for couples who have been having difficulty getting pregnant.
When most people think of infertility treatment, they think of IVF.
However, IUI is often suggested as the first line of treatment, as it’s much less invasive and less expensive than IVF.
So what happens during an IUI cycle? What should you expect?
However, IUI is often suggested as the first line of treatment, as it’s much less invasive and less expensive than IVF.
So what happens during an IUI cycle? What should you expect?
💌 🙏 Review your fertility doctor on our site! Takes less than 30 seconds but really helps other women who are getting started on their fertility journey! 💕
This article is a very in depth guide to the IUI process, so prepare yourself now!
We'll be covering:
👉the IUI process
👉cost of IUI
👉different IUI medications
👉IUI medication cost
👉IUI success rates by age, number of cycles, & diagnosis
After reading through this guide, you'll know what to expect for treatment.
So, what is IUI?
Intrauterine insemination (IUI) also known as artificial insemination, is a treatment used at fertility clinics to help a woman get pregnant by timing ovulation with an insemination procedure to give the sperm a better chance of reaching the egg while it is viable.
When an egg is released into the fallopian tube, there’s a short window of time when it can be successfully fertilized by a sperm, so it’s important to time the insemination as closely as possible to ovulation.
To put the IUI process simply:
👉 Your menstrual cycle is tracked to time ovulation. You may be prescribed medications to help stimulate your ovaries and time ovulation.
👉 On the day of ovulation, your partner will provide a semen sample at the clinic (or a vial of donor sperm is thawed if you're using a sperm donor). A doctor or nurse will perform the insemination, which is done using a catheter that releases the sperm sample into your uterus.
👉 Two weeks later, you'll go back in for a blood pregnancy test to see if the cycle was successful.
🕵️♀️ Find fertility clinics near you and get a consultation on whether IUI makes sense for you.
Who is IUI most successful for?
A reproductive endocrinologist, which is a fertility specialist, will take several factors into consideration when choosing the best method of treatment to help you get pregnant, which could include an IUI cycle.
Some women have a higher chance of success with IUI than others.
A lot of it can depend on your age and the type of infertility diagnosis you have.
Some women have a higher chance of success with IUI than others.
A lot of it can depend on your age and the type of infertility diagnosis you have.
Your treatment options can be dictated by several factors such as your age, infertility diagnosis, and the length of time you've been trying to conceive.
IUI is often recommended as the first line of treatment for:
- women < 38 years old
- unexplained infertility
- ovulatory dysfunction (e.g. PCOS)
- mild male factor infertility
- same-sex female partners
- single mother by choice
There are situations when your test results and your diagnosis will cause your doctor to recommend IVF over IUI.
It really depends on your unique situation.
IUI is also often recommended if fertility test results show a normal:
🙋♀️HSG (fallopian tubes are open)
🙋♂️Semen Analysis (normal sperm count, motility, and morphology)
🙋♀️HSG (fallopian tubes are open)
🙋♂️Semen Analysis (normal sperm count, motility, and morphology)
Why do these tests matter?
✅ HSG
A hysterosalpingogram (HSG) tests whether the fallopian tubes are open.
The test is done by injecting a special dye into the uterus which will travel into each fallopian tube and spill out by the ovary into the pelvic cavity, which can all be seen by x-ray.
The test is done by injecting a special dye into the uterus which will travel into each fallopian tube and spill out by the ovary into the pelvic cavity, which can all be seen by x-ray.
If your fallopian tubes are open, then an IUI is possible.
🙅♀️If the fallopian tubes are blocked or not present, the sperm would not be able to reach the egg through the IUI process.
Women that have tubal issues such as blocked or missing fallopian tubes would likely need to do IVF instead.
However, some women that have just one open fallopian tube do move forward with IUI.
However, some women that have just one open fallopian tube do move forward with IUI.
✅ Semen Analysis
Your partner's semen analysis results can also affect whether IUI is the best treatment option.
📈The number of motile sperm in a semen sample significantly affects IUI success rates.
IVF might be recommended over IUI if your partner's semen analysis shows:
- low sperm count
- low motility
- poor morphology
How does IUI work step by step?
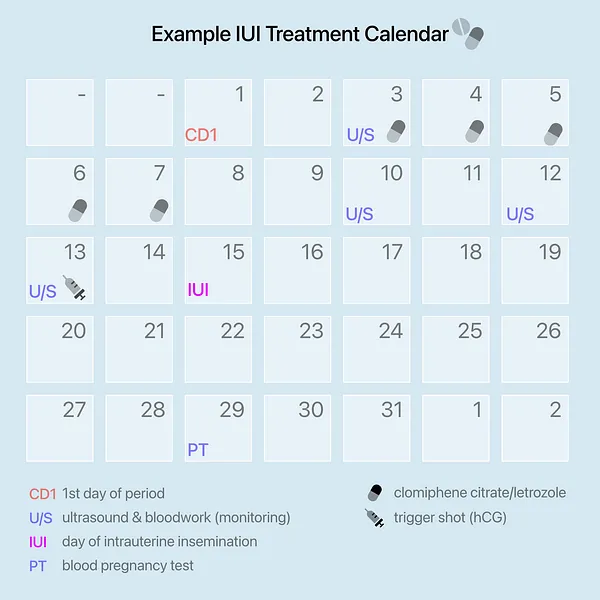
The timeline for an IUI cycle takes about 2 weeks from start to finish.
Short & sweet overview of the IUI process
- Fertility medications start around Day 2 or 3 of the menstrual cycle
- Fertility doctor monitors the growth of your follicles (in your ovaries) for ~10 days
- Once a follicle is large enough, you take a trigger shot to induce ovulation
- The IUI is scheduled ~36 hours after the trigger shot
- Two weeks later, you have a blood pregnancy test
💡Tip: Cycle Day 1 (CD1) is marked as the first day of your period with a full flow, not spotting.
The IUI process step-by-step:
- Call the clinic on the first day of your period (Cycle Day 1)
- Ultrasound & bloodwork is done on Cycle Day 2 or 3 to clear you to begin the IUI cycle
- Start taking fertility medications on Cycle Day 2 or 3
- Continue medications (5 days for oral medications or up to 13 days for injectable medications. This varies by medication type and your body’s response.)
- Bloodwork and ultrasounds are done every 2-3 days to make sure you are responding well to the medications and to track follicle growth
- Trigger shot is taken to induce ovulation once a follicle is large enough (diameter ≥18mm)
- IUI will take place ~36 hours after taking the trigger shot
- Andrology lab processes a fresh/frozen semen sample from your partner/donor (~1 hour)
- Insemination is performed by a nurse/doctor by inserting the sperm sample into your uterus using a catheter
- 2 weeks later, return to the clinic for a blood pregnancy test (beta hCG)
🕵️♀️ Ready to talk to a doctor about IUI? Head to our fertility clinic directory to find fertility doctors in your area, learn about each provider & view their success rates.
IUI Steps Explained
Why do I need to take medications for IUI? 🧐
The purpose of taking fertility medications for an IUI is to stimulate your ovaries to develop a follicle containing an egg.
Most patients will take either Clomiphene Citrate (Clomid) or Letrozole for an IUI cycle. These are both oral medications.
Most patients will take either Clomiphene Citrate (Clomid) or Letrozole for an IUI cycle. These are both oral medications.
During the follicular phase, the hypothalamus region of your brain releases GnRH which signals to the pituitary to release FSH (Follicle Stimulating Hormone) to stimulate your ovaries to grow a follicle.
Clomid and Letrozole work differently in the body but both send a signal to your brain that more FSH is needed, which further stimulates your ovaries to grow a follicle.
Clomid and Letrozole work differently in the body but both send a signal to your brain that more FSH is needed, which further stimulates your ovaries to grow a follicle.
In some cases, you might need more heavy-duty stimulation so instead of using either of these oral medications, they would use gonadotropins.
With gonadotropins, the goal is not to signal to your brain to produce FSH. Instead these medications actually contain FSH and are acting on the ovary directly to grow a follicle.
With gonadotropins, the goal is not to signal to your brain to produce FSH. Instead these medications actually contain FSH and are acting on the ovary directly to grow a follicle.
Sometimes these fertility medications cause the ovaries to work extra hard and you start growing 2 or more large follicles which each contain an egg, which could lead to a twin/triplet/etc pregnancy.
Because having multiple follicles growing during an IUI cycle puts you at a higher risk of having a multiple pregnancy, physicians try to avoid recruiting too many follicles for an IUI cycle.
A twin/triplet/etc pregnancy increases the risk of certain health issues for the mother and the babies, so physicians usually try to aim for just one healthy baby per cycle.
Because having multiple follicles growing during an IUI cycle puts you at a higher risk of having a multiple pregnancy, physicians try to avoid recruiting too many follicles for an IUI cycle.
A twin/triplet/etc pregnancy increases the risk of certain health issues for the mother and the babies, so physicians usually try to aim for just one healthy baby per cycle.
An IUI is typically cancelled if more than 3 follicles are growing as the risk of twins or triplets is too high.
Why do I need ultrasound & bloodwork appointments for IUI? 🧐
Monitoring helps your doctor time when the IUI should take place.
Your physician needs to monitor your progress prior to ovulation to make sure you are responding well to the medication protocol and that the optimal number of follicles are growing.
The amount of monitoring needed varies based on the clinic & your response to the medications.
The amount of monitoring needed varies based on the clinic & your response to the medications.
Your physician also needs to follow the development of your follicles in order to assess when you should take the trigger shot.
This is usually once the follicle size has reached ≥18mm.
This is usually once the follicle size has reached ≥18mm.
What is the trigger shot for in IUI? 🧐
During a normal menstrual cycle in the follicular phase, your brain releases FSH which signals to your ovaries to develop a follicle that contains an egg.
The follicle produces estradiol which increases as the follicle develops and gets larger.
Your brain continues to release FSH to continue to stimulate the follicle to grow.
Once the follicle is large enough, the high levels of estradiol being produced in your body signals to your brain to trigger ovulation by releasing a burst of LH, known as the LH surge.
The LH surge causes the egg to complete the maturation process and ovulation occurs about 24-48 hours later.
The follicle produces estradiol which increases as the follicle develops and gets larger.
Your brain continues to release FSH to continue to stimulate the follicle to grow.
Once the follicle is large enough, the high levels of estradiol being produced in your body signals to your brain to trigger ovulation by releasing a burst of LH, known as the LH surge.
The LH surge causes the egg to complete the maturation process and ovulation occurs about 24-48 hours later.
The trigger shot you take for an IUI cycle mimics this LH surge that normally occurs to induce ovulation.
Instead of containing LH, the trigger shot contains hCG, which has homology to LH and can act similarly in the body.
Instead of containing LH, the trigger shot contains hCG, which has homology to LH and can act similarly in the body.
👉Ovulation occurs about 36 hours after the trigger shot is administered.
Depending on your protocol, you might need to take a trigger shot to induce ovulation or you may just monitor for your body's natural LH surge, which can be done ether at the clinic or at home with ovulation test strips.
How is the semen sample prepared for IUI?
On the day of the IUI, either your partner will provide a fresh semen sample to the lab or your frozen vial of donor/partner sperm will be thawed and processed.
The semen sample is processed in order to remove any immotile sperm and leave only the motile sperm that would be able to travel through your uterus to reach the egg.
The semen sample is processed in order to remove any immotile sperm and leave only the motile sperm that would be able to travel through your uterus to reach the egg.
This gives the sperm that can move a better chance of moving through the uterus.
A sample containing a high percentage of immotile sperm can sometimes create a mesh-like structure making it difficult for the motile sperm to navigate out of.
A sample containing a high percentage of immotile sperm can sometimes create a mesh-like structure making it difficult for the motile sperm to navigate out of.
The sperm processing takes about 1 hour.
Once the IUI sample is ready, a nurse or reproductive endocrinologist will use a catheter to insert the sperm sample into your uterus.
The Two-Week Wait
A blood pregnancy test will be done at the clinic about 2 weeks after your IUI in order to assess whether your cycle was successful.
A beta hCG level of >5 mIU/mL indicates a positive pregnancy.
A beta hCG level of >5 mIU/mL indicates a positive pregnancy.
How much does IUI cost?
Let’s get right down to the financial aspects of intrauterine insemination.
The cost of IUI varies based on:
👉 your fertility clinic
👉 insurance coverage
👉 monitoring appointments - whether you will track ovulation at the clinic or at home
👉 the number of monitoring visits needed
👉 type of fertility medication you take
👉 your fertility clinic
👉 insurance coverage
👉 monitoring appointments - whether you will track ovulation at the clinic or at home
👉 the number of monitoring visits needed
👉 type of fertility medication you take
On average, an IUI cycle costs $2500.
That's not including medications but for the majority of women, IUI medications are inexpensive.
That's not including medications but for the majority of women, IUI medications are inexpensive.
Here’s the cost breakdown for a medicated IUI cycle:
- monitoring appointments for bloodwork & ultrasounds ($1500)
- sperm preparation & insemination procedure ($1000)
- IUI medications ($170-$2700; see later in this article for our medication cost table)
💊 Wondering why the medication range is so large?
We made you an IUI medication cost table later in this article that explain the cost of different medications you could be prescribed!
🕵️♀️ Ready to start looking for a fertility clinic? Head to our fertility clinic directory to find fertility doctors in your area, learn about each provider & view success rates by fertility clinic.
What's the cost of IUI with insurance?
The numbers above are good estimates for women who are self-paying and not using insurance.
To figure out how much an IUI costs with insurance, you need to know some specific details about your health insurance plan, such as the deductible and your co-insurance.
Check out our infertility insurance guide on how to calculate the cost of infertility treatment with insurance.
In that article we use IVF as the example for the calculations, so you would just sub in your IUI expenses instead to calculate what you would expect to pay.
IUI medication protocols
There are two main types of treatment protocols:
- natural IUI cycles 🌺
- medicated IUI cycles 💊
IUI without medication - Natural Cycle 🌺
Patients don’t always take fertility drugs for an intrauterine insemination cycle.
If you will not be using fertility medications, it is called a natural cycle.
In this case your doctor will follow your body’s natural menstrual cycle & hormone fluctuations to monitor follicle growth and will time the IUI for when your body ovulates on its own.
IUI with medication 💊
Medications are needed for women who do not ovulate on their own or who have irregular cycles.
But this protocol is also used for women who have regular cycles as well to increase their chances of success with intrauterine insemination.
But this protocol is also used for women who have regular cycles as well to increase their chances of success with intrauterine insemination.
Fertility medications allow for more control over the timing of ovulation and can encourage one to two follicles (each containing an egg) to develop to increase chances of pregnancy.
There are 3 common types of medications used for IUI:
👉Clomiphene Citrate (e.g. Clomid)
👉Letrozole (e.g. Femara)
👉Gonadotropins (e.g. Gonal-F, Follistim, etc.)
👉Clomiphene Citrate (e.g. Clomid)
👉Letrozole (e.g. Femara)
👉Gonadotropins (e.g. Gonal-F, Follistim, etc.)
Your doctor will prescribe one of these medications for your IUI treatment.
They also may prescribe you a trigger shot (hCG) to induce ovulation.
Some women will not need a trigger and their body's natural LH surge will induce ovulation.
They also may prescribe you a trigger shot (hCG) to induce ovulation.
Some women will not need a trigger and their body's natural LH surge will induce ovulation.
How much do IUI medications cost?
We did some research on the self-pay rates for each medication type for a typical IUI cycle.
We factored in the dosage & average number of days medications are taken for intrauterine insemination.
We factored in the dosage & average number of days medications are taken for intrauterine insemination.
We put it all in this table for you 😘
Oral medications like Clomid and Letrozole are fairly inexpensive, while injectable gonadotropins are the most expensive medication type for an IUI.
Note that while Clomid/Letrozole are only taken for 5 days, gonadotropins are taken for longer, with the average being about 10 days of injections.
IUI Success Rates
The success rates of an IUI depend on several different factors. Once your initial fertility testing is complete, your your physician should be able to give you estimates that are specific to your chances of getting pregnant from a cycle.👩⚕️💬
IUI can have fairly low success rate per cycle but they’re higher than trying to conceive naturally for couples experiencing infertility.
The success rate of an IUI cycle is typically anywhere between 5%-20% depending on several different factors such as total motile sperm count and female age.
We'll take a look at these different factors below to see how they affect success rates.
The success rate of an IUI cycle is typically anywhere between 5%-20% depending on several different factors such as total motile sperm count and female age.
We'll take a look at these different factors below to see how they affect success rates.
How many IUI should I do before considering IVF?
Fertility doctors typically suggest a minimum of 3 IUI cycles before considering alternative treatment, such as in vitro fertilization.
However, the recommended number of IUIs can change depending on your age and diagnosis.
🕵️♀️ Ready to start looking for a fertility clinic? Head to our fertility clinic directory to find fertility doctors in your area, learn about each provider & view their success rates.
IUI Success Rates Differ by Diagnosis
A 2020 review of factors that affect IUI success rates found that diagnosis does affect which couples are likely to have success in just a few cycles.
One study including patients of all diagnoses showed the success rate after just the first IUI cycle was 16.4%.
Clinical pregnancy rates do increase over a few cycles depending on different factors.
Patients with ovulatory disorders such as PCOS have shown the highest success rates with IUI compared to other diagnoses.
IUI Success rates after a maximum of 4 cycles using Clomid were:
- 46% for ovulatory dysfunction (such as PCOS)
- 38% for cervical factor/male factor/unexplained infertility
- 34% for endometriosis
- 26% for tubal factor
IUI Success Rates Over 40
Female age is also known to significantly affect IUI success rates. As women get older, their chances of success with IUI decrease.
One large study on IUI success rates found low pregnancy rates for women over 40:
- 11.1% to 18.9% per IUI cycle for women < 40 years old
- 4.7% per IUI cycle for women 40-45 years old
Women that are 40 years or older are typically advised to do IVF as their chance of success with IUI is much lower.
IUI Success Rates for Low Sperm Count
The severity of male factor infertility can also significantly affect the IUI outcome.
Specifically, the number of motile sperm in a semen sample has been shown to affect IUI success rates.
How many sperm is ideal for IUI?
A review of the scientific literature found that IUI is ideal when there's at least 5-10 million total motile sperm in the semen sample.
The WHO sets criteria for what is considered to be a normal semen sample.
A sample is considered abnormal if the semen sample has a:
👉 sperm concentration < 15 million/mL
👉 total sperm count < 39 million
👉 total motile sperm < 40%
👉 progressively motile < 32%
👉 normal sperm morphology < 4%
So, roughly 15.6 million total motile sperm would be considered the lower threshold for a normal semen sample.
A large clinical trial sub-analysis of 2,462 cycles found that while it was difficult to identify how many sperm is too few, it was clear that a higher total motile sperm count was associated with increased clinical pregnancy rates.
- 15-20 million total motile sperm resulted in a 14.8% live birth rate
- <5 million total motile sperm resulted in a 5.5% live birth rate
What about sperm morphology?
Typically if a semen analysis shows a low sperm morphology, reproductive endocrinologists are inclined to recommend IVF.
Typically if a semen analysis shows a low sperm morphology, reproductive endocrinologists are inclined to recommend IVF.
However, recent studies have found that sperm morphology is not a significant factor for IUI success rates and a recent study concluded that a low sperm morphology should not preclude couples from trying IUI first if they wish.
IUI Success Rates with Letrozole vs Clomid
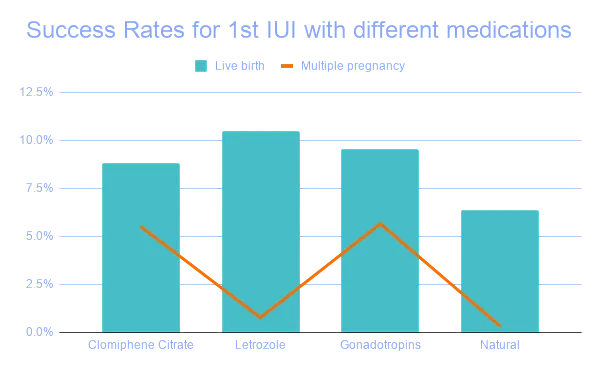
Although a cycle without medications can be an option for women that have a regular menstrual cycle, a recent study of 8,583 couples with either unexplained infertility or mild male factor infertility showed that using fertility medications for IUI significantly increases chances of pregnancy in these groups.
For patients in their first IUI cycle, the live birth rate of an unmedicated cycle was 6.4% while medicated cycles averaged 9.4%.
The best performing medication protocol was Letrozole.
Women that took Letrozole for their IUI cycle showed comparable live birth rates to the other medication options (10.5%) but had the lowest incidence of twins/triplets/etc. (0.8%).
The goal of an IUI is to provide the highest success rates while keeping the incidence of multiple gestations (twins, triplets, etc) as low as possible to ensure the best health & safety for the mother and baby.
What if the first IUI doesn't work?
As success rates for IUI aren't very high per cycle, some women may need to do multiple rounds of IUI in order to get pregnant.
Let's take a look at the success rates beyond the first IUI cycle.
IUI Success Rates after 3 Cycles
Most reproductive endocrinologists will suggest that a patient tries at least 3 IUI cycles before considering any more invasive or expensive treatment.
The study of couples with unexplained or mild male factor infertility reported that cumulative success rates after 3 IUIs for medicated cycles resulted in a live birth rate of roughly 25%.
Source: Huang et al., 2018
After 3 failed IUI cycles, your physician may recommend that you consider moving to in vitro fertilization as the success rates of IVF per cycle are much higher.
IUI Success Rates for PCOS
Women diagnosed with ovulatory dysfunction, such as polycystic ovarian syndrome (PCOS), have been associated with the highest cumulative pregnancy rates after IUI when compared to women with other diagnoses.
A large study of women with ovulatory disorders using Clomid with IUI resulted in a cumulative clinical pregnancy rate of 46% after 4 IUIs.
IUI with Letrozole vs Clomid for PCOS
Studies have found that when it comes to patients with PCOS, there’s a difference in which medication performs the best for IUI/ovulation induction.
A review of 42 randomized controlled trials with a total of 7,935 patients undergoing IUI or timed intercourse found that Letrozole has better success rates for women with PCOS than Clomid.
A 2019 review also found that Letrozole improved ovulation, pregnancy rates, and live birth rates for women with PCOS compared to Clomid and had lower risk of multiple gestation.
What about injectable medications?
Gonadotropins also showed higher pregnancy and live birth rates for women with PCOS compared to Clomid, with one study reporting a pregnancy rate of 47.7% per couple.
However, the number of cycles for the couples in this study ranged from 1-9 and a per cycle breakdown for this patient group was not provided.
However, the number of cycles for the couples in this study ranged from 1-9 and a per cycle breakdown for this patient group was not provided.
While gonadotropins provide a higher success rate than Clomid, there is an unacceptably high rate of twins/triplets/etc and an increased risk of Ovarian Hyperstimulation Syndrome (OHSS).
Because of this, gonadotropins are not commonly recommended for IUI. The cost of these medications is also much higher than other options.
Because of this, gonadotropins are not commonly recommended for IUI. The cost of these medications is also much higher than other options.
How do I find a fertility clinic for IUI?
To find fertility clinics in your area that offer intrauterine insemination, head to our fertility clinic directory to research your options.
There you can search by your city or the name of a doctor/clinic where you can get initial fertility testing done and discuss whether fertility treatments makes sense for you.
Check each clinic profile for options in your area and have a look at the success rates, number of doctors, locations they have, and their contact info.
Then give them a call to learn a bit more about scheduling a consultation with one of their doctors!
Not sure how to choose which fertility clinic to reach out to?
Read out guide on how to choose the best fertility clinic to get the 5 criteria you should take into account when comparing which clinic and doctor makes sense for your unique needs.
Are you preparing for an IUI cycle?
If you’re planning on IUI, what is the success rate your doctor gave for your age/diagnosis?
Head to our instagram account for weekly tips, tricks, and support and to find others who are going through the process.
Always remember, #iuigotthis.
Always remember, #iuigotthis.
🕵️♀️ Ready to start looking for a fertility clinic? Head to our fertility clinic directory to find fertility doctors in your area, learn about each provider & view their success rates.