Guides
PGT-A: Guide to Preimplantation Genetic Testing of Embryos in IVF

What is PGS/PGT-A for IVF?
Genetic testing of embryos as part of an IVF cycle has hugely increased in popularity over the past few years, with 44% of all embryo transfers including an embryo tested by PGT in the United States in 2019, up from 38% in 2018.
If you're considering having your embryos tested through PGT-A, you likely have some questions about what this test even is and how it works.
Here, we'll discuss all the common questions and misconceptions regarding genetic testing of embryos by PGT-A.
Do you like your fertility doctor? 💌 🙏 Review your fertility clinicon our site! Other women need your opinion to help them choose a great fertility provider!
What does PGT-A stand for?
PGT-A stands for preimplantation genetic testing for aneuploidy.
This is a fancy way of saying that it tests whether an embryo has the correct number of chromosomes before it has been transferred back into the uterus to attempt a pregnancy.
So this test can help doctors and IVF patients choose the best possible embryo that is most likely to result in a successful pregnancy.
PGT-A vs PGS
You may have heard both of these terms concerning the genetic testing of embryos, PGT-A and PGS. Let’s clear up the confusion between these two terms.
PGT-A and PGS are the exact same test!
PGT-A is the new name for the test and PGS is the old name.
PGS stands for preimplantation genetic screening and also tests how many chromosomes an embryo’s cells contain.
PGS was renamed to PGT-A in 2016. As the test name was only changed in the past few years, a lot of people still refer to the test as PGS, even though the official name is now PGT-A.
Preimplantation genetic screening (PGS) is a certainly less descriptive name than preimplantation genetic testing for aneuploidy (PGT-A). With the new name, it's more obvious what the test is screening for.
💌 🙏 Review your fertility doctoron our site! Takes less than 30 seconds but really helps other women who are getting started on their fertility journey! 💕
What is PGT-A? How does it work?
Ok, so let's dive into what PGT-A actually tests for and how it works.
Humans need to have 23 pairs of chromosomes (46 in total) in their cells in order to be viable and lead to a healthy baby. Those chromosomes are named 1-22 for which there is a matching pair for each and then you have two sex chromosomes, either XX or XY.
When an embryo’s cells have an incorrect number of chromosomes, either too few or too many, it's known as aneuploid. This is an abnormal result.
An embryo that has the correct number of chromosomes is referred to as euploid. This embryo would be considered normal and safe to transfer.
A PGT-A report of an embryo will either result in a normal embryo, where its cells have 46 chromosomes (23 pairs), an abnormal embryo where it has extra or missing chromosomes, or a mosaic embryo in which some cells of the embryo are normal and some are abnormal.
PGT-A result types:
- Euploid embryos (all cells are normal)
- Aneuploid embryos (all cells are abnormal)
- Mosaic embryos (some cells are normal and some are abnormal)
As PGT-A identifies the presence of all chromosomes, it can tell you whether an embryo is male or female (XY vs XX) and can also indicate chromosomal abnormalities.
If an embryo is aneuploid, it most commonly will result in either fail to implant or the embryos will not be able to develop past a certain stage and will result in a miscarriage.
There are however, a few instances in which an embryo with an extra chromosome or a missing chromosome can lead to a live birth of a baby. One such example is Down Syndrome.
Does PGT-A test for Down Syndrome?
Although most whole chromosome abnormalities cannot lead to a viable embryo, there are instances in which an embryo with an abnormal number of chromosomes can lead to life.
The most commonly known example would be Down Syndrome, in which the embryo’s cells have an extra copy of Chromosome 21, referred to as Trisomy 21 because there are three copies of the chromosome present as opposed to just the two copies.
An embryo affected by Down Syndrome would result as abnormal from PGT-A showing a result like:
Abnormal female embryo: 47 XX, +21
Abnormal male embryo: 47 XY, +21
A normal embryo should be 46 XX or 46 XY, so in this case, the result would show that there is one extra chromosome present, an additional Chromosome 21.
As PGT-A tests for the number of chromosomes in an embryo’s cells and the identity of each chromosome, the results can identify embryo’s affected by Down Syndrome.
Preimplantation genetic testing for aneuploidy can also identify other full chromosome genetic abnormalities such as Monosomy X, known as Turner Syndrome, in which an embryo just has one sex chromosome, indicated as XO, as opposed to having a pair of sex chromosomes, XX or XY.
What happens to my embryos when using PGT-A?
First important thing to know, is that your embryos do not leave the embryology lab at your clinic.
Some patients worry that if they choose to do PGT-A, their embryos will be sent off to a reference lab to be tested. That's not the case at all.
Instead, just a biopsy of the embryo is sent for testing.
On Day 5 or Day 6 of embryo development once an embryo has developed to the blastocyst stage, an embryologist removes a few cells from the embryo.
This is known as an embryo biopsy and is sent off to a genetics lab for PGT-A.
On Day 5 or Day 6 of embryo development once an embryo has developed to the blastocyst stage, an embryologist removes a few cells from the embryo.
This is known as an embryo biopsy and is sent off to a genetics lab for PGT-A.
In the meantime, the embryos are frozen and stored in the embryology lab at your clinic while you await the test results. So your embryos don’t go anywhere!
PGT-A Process & Timeline
- Day 0 eggs are fertilized in the embryology lab
- Day 5 embryos that have reached the blastocyst stage are biopsied, slow developing embryos are checked again the next day
- Day 6 any embryos that were not ready on Day 5 but have now developed to the blastocyst stage are biopsied
- Day 6+ biopsy samples are sent to the genetics lab for testing
- Day 18+ PGT-A results come back indicating which embryos are normal/abnormal/mosaic
Ok, so how does the biopsy work?
💌 One day you will tell your story of how you've overcome what you're going through now, and it will become part of someone else's survival guide.
Please take 5 minutes to REVIEW your fertility doctor! It helps other patients just beginning find the best doctor for their needs.
PGT-A Biopsy
During IVF, eggs are fertilized to create embryos which are usually then cultured in the embryology lab for 3 to 6 days. During this time, embryologists can monitor the development of each embryo to see whether they are developing normally.
Not all embryos will usually make it to Day 5 or 6. Some embryos will not divide normally and will stop developing. However, some aneuploid embryos can still continue developing to Day 5 or 6 and appear normal.
It is most common for IVF patients to wait until their embryos are at either Day 5 or Day 6 of development before testing them.
Embryos will have grown to the blastocyst stage by Day 5 or 6 of development.
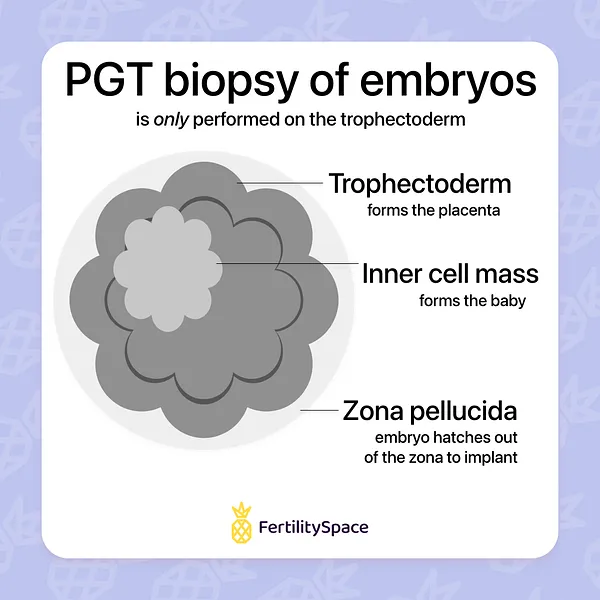
It is now common practice to wait to test embryos until they have developed to the blastocyst stage because at this point, the embryo has two distinct cell types, an inner cell mass and the trophectoderm.
This makes it safer to test embryos because you can now distinctly tell the difference between the cells that will form the actual baby, called the inner cell mass, and the cells that will form the placenta, known as the trophectoderm.
Inner cell mass = baby
Inner cell mass = baby
Trophectoderm = placenta
For the PGT-A biopsy, only cells from the trophectoderm (which forms the placenta) are removed and sent for testing.
The cells that will form the baby are left intact and are not used for testing.
Ok, so how does the embryologist remove the cells?
The embryologist uses a large pipette with light suction to hold the embryo in place.
From the other side of the embryo, a large aspirating pipette will tease out 5-7 cells of the trophectoderm and free them from the blastocyst using small laser pulses.
From the other side of the embryo, a large aspirating pipette will tease out 5-7 cells of the trophectoderm and free them from the blastocyst using small laser pulses.
The cell biopsy is then sent off to the genetics lab where it can be tested for how many chromosomes are present in these cells.
Some patients ask whether the removal of some pre-placental cells will affect the implantation of the embryo.
A recent study of frozen embryo transfer cycles found that there was no difference in implantation rates amongst patients doing their first IVF cycle who had their embryos biopsied for PGT-A (47.9%) versus an age-matched control group that did not have their embryos biopsied (45.8%).
How accurate is PGT-A?
PGT-A has been reported to have a high accuracy rate of about 98%.
A 2021 study on preimplantation genetic testing for aneuploidy of 484 FET cycles found that for couples doing their first ever IVF cycle and tested their embryos by PGT-A, the clinical error rate was 0% for the tests ability to predict an aneuploid embryo.
Meaning that the PGT-A results were very accurate in predicting which embryos would not lead to a successful pregnancy due to aneuploidy.
What can PGT-A results tell you about your embryos?
OK, so let’s talk about what these results can and cannot tell you about your embryos and chance of conceiving from a transfer cycle.
PGT-A results can identify:
- which embryos are chromosomally abnormal (aneuploid)
- which embryos are normal (euploid) and likely to lead to a healthy baby
- the sex of the embryo (male vs female)
PGT-A can tell you with a high accuracy whether an embryo’s cells have the correct number of chromosomes.
This information can help you select the embryo that is most likely to result in a successful pregnancy and live birth. However, a PGT-A normal embryo does not guarantee a successful transfer cycle.
Even with this extra testing information, a PGT-A normal embryo is estimated to have a 60% chance of live birth from a transfer cycle.
It’s important to keep in mind that, while preimplantation genetic testing can help improve your odds of getting pregnant from a transfer cycle, it’s still not a 100% guarantee that your transfer will be a success.
As preimplantation genetic testing results tell you which chromosomes an embryo’s cells contain, the test results can tell you the sex of the embryo as well (male vs female).
However, the test cannot tell you anything about the baby’s physical traits, such as eye or hair color.
Does age affect how many normal embryos you will get from IVF?
So you may be wondering, what your chances are of your embryos being normal?
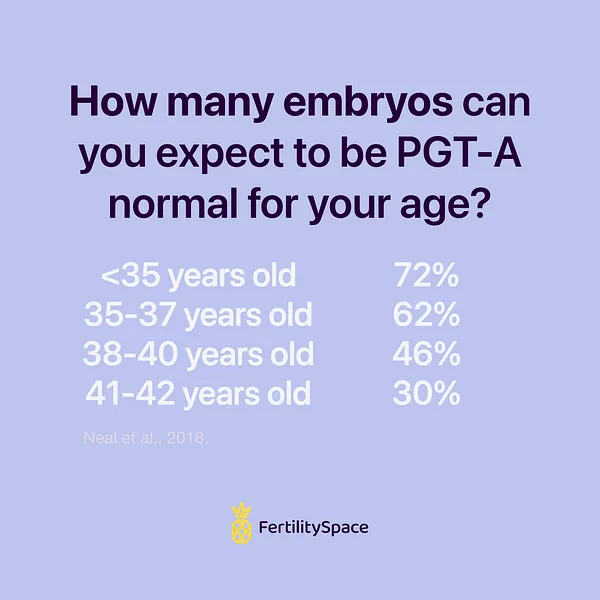
A big factor is maternal age at the time that the eggs are retrieved in the IVF cycle.
As female age increases, fertility declines.
A large part of the decline in fertility is due to the decreased ability of the egg to function correctly which can lead to incorrect cell division resulting in some cells having too many chromosomes and some too few.
Younger women have a higher likelihood of generating normal embryos from an IVF cycle while older women tend to have a high prevalence of abnormal embryos.
This is one big reason why some women end up having to use donor eggs from a younger woman, to mitigate the age-related decline of egg quality.
You can take a look at the the success rates using donor eggs in our article looking at the national data fro IVF success rates when using an egg donor.
Older women can still use their own eggs and have a successful IVF cycle but they will likely have a lower number of normal embryos available and it may take more than one cycle to get a normal embryo, it depends.
There has been data published that can give you an idea of your chances of getting normal embryos based on your age at the time of egg retrieval.
You can take a look at the the success rates using donor eggs in our article looking at the national data fro IVF success rates when using an egg donor.
Older women can still use their own eggs and have a successful IVF cycle but they will likely have a lower number of normal embryos available and it may take more than one cycle to get a normal embryo, it depends.
There has been data published that can give you an idea of your chances of getting normal embryos based on your age at the time of egg retrieval.
A recent study of almost 9,000 patients having their embryos tested by PGT-A found that there was a clear increase in abnormal embryos as female age increased.
The prevalence of chromosomally normal embryos decreases as women get older:
Success rates when transferring a PGT-A normal embryo
OK, so you know on average the percent of normal embryos you’re likely to get from an IVF cycle.
But once you have a PGT-A normal embryo, what is the success rate for getting pregnant and having a baby from the frozen embryo transfer cycle?
The current literature estimates that the transfer of a PGT-A normal embryo on average has a 60% chance of live birth.
You may be wondering, does my age affect the success of the frozen embryo transfer even if I use a PGT-A normal embryo?
It is known that female age at the time the egg is retrieved impacts the likelihood that an embryo will be chromosomally normal however, there have been conflicting results on whether female age at the time of transferring a viable embryo impacts clinical outcomes.
A 2020 study of 8175 single euploid frozen embryo transfer (FET) cycles found that the female age has a significant affect on embryo transfer outcomes, specifically implantation, clinical pregnancy, and live birth rates.
Here’s the data on the difference in live birth rates of PGT-A normal embryos by the age of the female patient at the time of her frozen embryo transfer.
While PGT-A does give you helpful data on which embryos from an IVF cycle are most likely to lead to a healthy baby, it’s not a guarantee that the transfer will be a success.
Implantation rates were affected by:
- Female age
- AMH level
- Day of embryo transfer
- Embryo morphology
When controlling for these other confounding factors to just look at the effect of maternal age, the study found that only implantation rate seems to be significantly affected by age.
Once successful implantation has occurred as signified by a positive beta hCG (pregnancy test), the progression to a clinical pregnancy and then to a live birth was not significantly different between ages.
Once successful implantation has occurred as signified by a positive beta hCG (pregnancy test), the progression to a clinical pregnancy and then to a live birth was not significantly different between ages.
For each age group in the study, roughly 80% of implanted pregnancies progressed to a clinical pregnancy, and roughly 90% of clinical pregnancies resulted in a live birth.
So once you are pregnant from transferring a PGT-A normal embryo, being older doesn’t appear to make you more susceptible to miscarriage compared to younger women, it instead impacts the initial hurdle of becoming pregnant and getting to that first positive pregnancy test.
If you're interested in checking out more IVF success rate data, you can check out our IVF Success Rates by Age article where we break down the newest CDC data to show you success rates for all IVF cycles from the most recent reporting year, success rates of new patient's for their first ever IVF cycle, embryo transfer success rates (regardless of PGT use), and donor egg IVF outcomes as well.
If you're interested in checking out more IVF success rate data, you can check out our IVF Success Rates by Age article where we break down the newest CDC data to show you success rates for all IVF cycles from the most recent reporting year, success rates of new patient's for their first ever IVF cycle, embryo transfer success rates (regardless of PGT use), and donor egg IVF outcomes as well.
How much does PGT-A cost?
You should expect to pay a few thousand dollars to have your embryos tested by PGT-A. The general range is $1650-$3750 but, like most things, it varies.
The cost of testing your embryos depends on a few factors, such as:
- clinic cost for the embryo biopsy
- genetics lab that is used for testing
- number of embryos tested
Want specifics?
Take a look at our full article on the cost of PGT-A and how to decide if it’s worth it for you.
We break down the cost for testing and show you the data on how your age can affect whether this extra testing cost is worth it by saving you time to pregnancy and money throughout treatment.
👋 Other patients want your input! Review your fertility doctor & clinic on our site to help future patients like you. Select your clinic & tell us what you think. It takes 5 minutes!
PGT-A CPT code
Ok, why are we giving you a CPT code?
Because you might want to double-check with your health insurance if they cover PGT-A for your specific diagnosis. Your medical plan will need to know the CPT codes for the testing procedures in order to assess whether it is covered under your plan.
They may also ask for your diagnosis code as well, so you’ll need to ask your clinic for which ICD-10 code that they would use for you when submitting claims to your insurance plan.
Most insurance companies do not cover preimplantation genetic testing. It’s usually an expense that the patient pays to the lab themselves, but it’s always good to check.
There are two different CPT codes for the embryo biopsy depending on how many embryos are being tested.
Embryology Lab CPT Codes
89290 - biopsy for PGT of <= 5 embryos
89291 - biopsy for PGT of > 5 embryos
Genetics Lab CPT Codes
88299 - molecular cytogenetics (used to code for PGT-A although there may be other variations your lab may use)
If you do end up paying for PGT-A yourself because your insurance won’t cover it, consider tracking this expense amount and receipt in case you can deduct it on your taxes for the year.
If you plan to itemize your taxes, you can deduct uninsured medical expenses related to IVF that exceed a certain percentage of your income.
We made you a guide on how to calculate whether deducting your IVF expenses makes sense for you and how to do it.
We even made you a free IVF expense tracking template that you can use to keep organized with your treatment costs throughout the year. You can find that link to that resource in our IVF tax deduction article.
Are you doing PGT-A/PGS?
Choosing whether or not to do preimplantation genetic testing is a total personal choice and is oftentimes left up to the patient to decide. It is an added expense and there is a small error rate in testing but it can help you to avoid paying for an embryo transfer that is highly likely to result in a failed cycle.
Do you think it’s worthwhile to test your embryos prior to choosing one to transfer or not?
Check out the most recent National IVF Success Rates by age in the United States.
Check out the most recent National IVF Success Rates by age in the United States.
👋 Your story matters! Want to use your experience to help others find a fertility provider? Leave an anonymous review of your fertility doctor & clinic.
.png)