Finance
IVF insurance laws by state
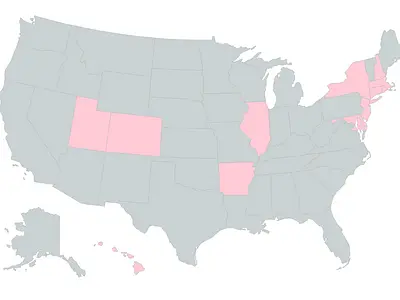
These 13 US states shaded pink require insurers to cover IVF
Ah, the holy grail of insurance plans, IVF coverage. Men and women alike have searched for this elusive line of text in their health plan documents for years only to find out that their employer doesn't provide infertility coverage, even if they live in a state that has infertility insurance laws!
So let's answer your primary question first. Which states mandate IVF coverage? There are currently 13 states that require insurance companies to cover IVF.
States that Cover IVF:
So let's answer your primary question first. Which states mandate IVF coverage? There are currently 13 states that require insurance companies to cover IVF.
States that Cover IVF:
- Arkansas
- Colorado
- Connecticut
- Delaware
- Hawaii
- Illinois
- Maryland
- Massachusetts
- New Hampshire
- New Jersey
- New York
- Rhode Island
- Utah
If you live in one of these states, read on for details regarding:
- what your states covers
- who can be covered for IVF
- how much your state will cover for IVF treatment
How do you know whether you can take advantage of this infertility coverage?
What You Should Know About IVF Coverage in Your State
To understand whether you can take advantage of your state laws, there are three basic questions we need to answer:
1. Does my state mandate that insurers cover IVF?
There are 19 states that have infertility insurance laws in place. Some of these states, such as California and Texas, only require insurers to offer infertility coverage to employers.
In this case it’s an optional benefit and your employer decides whether their employees will have a medical plan that includes infertility coverage.
Then there are states such as Louisiana and Ohio, which have infertility laws in place but do not require coverage for IVF specifically, so maybe you have insurance coverage for IUIs but not IVF.
In this case it’s an optional benefit and your employer decides whether their employees will have a medical plan that includes infertility coverage.
Then there are states such as Louisiana and Ohio, which have infertility laws in place but do not require coverage for IVF specifically, so maybe you have insurance coverage for IUIs but not IVF.
13 states require insurers to cover IVF as part of their health plans 🙌
These states often include specific requirements in their statutes for the infertility treatments and testing that insurers need to cover in their health plans.
Some states also set a limit for the maximum amount an insurer has to cover for each enrollee. This maximum may be set as a specific number of IVF cycles or as a max dollar limit that insurance companies have to cover for treatment.
These are lifetime maximums which means that after a patient has hit their limit, they won't be able to have any further treatment covered, instead they'd have to pay for it all themselves.
2. Is my employer fully-insured or self-insured?
Not all employers are required to comply with state IVF laws (keep that in mind before you burst into your HR thinking you've uncovered a conspiracy to avoid state law).
If your employer is fully-insured and uses a large group health plan, their health plans will comply with state mandates for IVF coverage.
If your employer is fully-insured and uses a large group health plan, their health plans will comply with state mandates for IVF coverage.
❗Self-insured employers are not required to follow state mandates for IVF coverage
That's not to say that they won't, self-insured employers still like to be competitive with the benefits they offer in order to attract the best talent to their company. Because they don't have to follow the state requirements, their coverage limits might even be better than what the state requires.
Small group employers, religious employers, and/or certain governmental programs are usually not required to comply with IVF coverage laws.
3. Do I meet the patient requirements to utilize IVF coverage?
Many of the states with IVF laws list requirements that a patient must meet in order to access IVF coverage.
This can be a number of things such as your age, duration of infertility, or insurers often require that your try a less expensive treatment covered under the plan first, like IUI, before you go to IVF.
This can be a number of things such as your age, duration of infertility, or insurers often require that your try a less expensive treatment covered under the plan first, like IUI, before you go to IVF.
Check out your state below for an overview of IVF coverage, how much can be covered, and who can use it.
Don't have IVF coverage mandated in your state?
If your employer doesn't offer coverage for infertility treatment, the cost of IVF can be fairly prohibitive.
However, there are ways that you can prepare yourself financially ahead of time to better handle some of the cost.
Check out our guide for tips on affording IVF treatment.
States that Mandate IVF Coverage Under Insurance
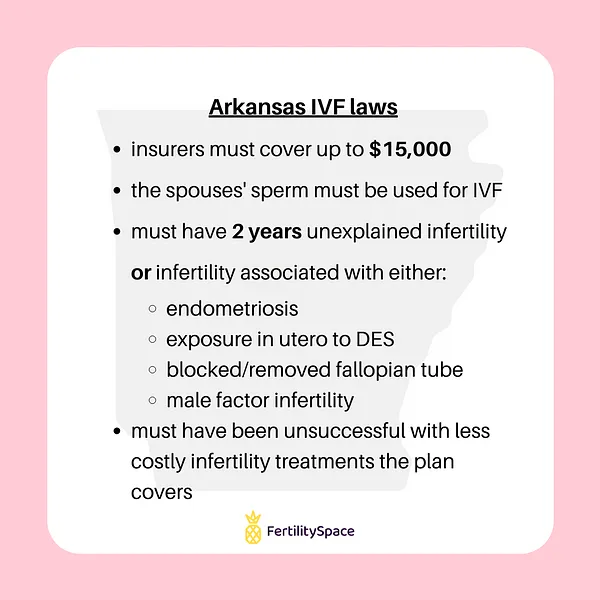
Arkansas
Akansas IVF Coverage Limit: $15,000 lifetime maximum coverage
Fertility Clinics in Little Rock, Arkansas
Fertility Clinics in Little Rock, Arkansas
Requirements for IVF coverage
- the patient and patient’s spouse have unexplained infertility for at least 2 years or
- infertility associated with a medical condition of:
- endometriosis
- exposure in utero to diethylstilbestrol (DES)
- blockage or removal of one/both fallopian tubes
- abnormal male factors contributing to infertility
- the patient's oocytes are fertilized with the sperm of the patient's spouse
- procedures are to be performed at medical facilities that conform to the standards and guidelines of ASRM or ACOG
- the patient has been unable to obtain successful pregnancy through any less costly applicable infertility treatment for which coverage is available under the policy
IVF Coverage in Arkansas includes
- $15,000 lifetime maximum
- in vitro fertilization (IVF)
- embryo cryopreservation (embryo freezing)
Egg/sperm freezing coverage
None listed.
Insurance carrier limitations on coverage
- IVF coverage applies to insurance plans that offer pregnancy-related benefits.
- Deductibles, co-insurance, and out-of-pocket limitations for infertility must be the same as provided under pregnancy-related benefits.
- Limitations on coverage due to a pre-existing condition should not exceed a period of 12 months.
Employers that are exempt from state law
Self-insured employers.
Read the Arkansas IVF State Laws
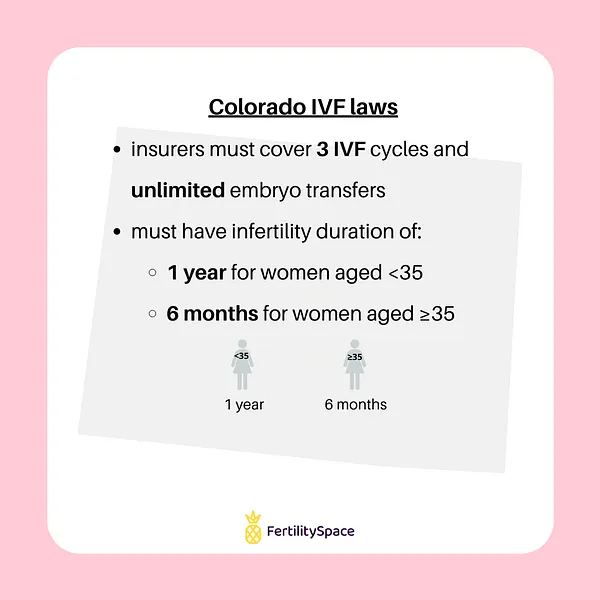
Colorado
Colorado IVF Coverage Limit: 3 IVF cycles and unlimited embryo transfers
Fertility Clinics in Denver, Colorado
Fertility Clinics in Denver, Colorado
Requirements for IVF coverage
- infertility defined as the failure to conceive or successfully carry a pregnancy after either
- 12 months of regular, unprotected sexual intercourse for a women under 35
- 12 months of therapeutic donor insemination for a woman under 35
- 6 months of regular, unprotected sexual intercourse for a woman aged 35 or older
- 6 months of therapeutic donor insemination for a woman aged 35 or older
- a person's inability to reproduce either as an individual or with the person's partner or
- a licensed physician's findings based on a patient's medical, sexual, and reproductive history, age, physical findings, or diagnostic testing
IVF Coverage in Colorado covers
- 3 completed oocyte retrievals
- unlimited embryo transfers (using single embryo transfer when recommended and medically appropriate)
Egg/sperm freezing coverage
Covered for a person who has a medical condition or is expected to undergo medication therapy, surgery, radiation, chemotherapy, or other medical treatment that is recognized by medical professionals to cause a risk of impairment to fertility.
Insurance carrier limitations on coverage
- Exclusions, limitations, or other restrictions on coverage of fertility medications shall not differ from those imposed on any other prescription medications covered.
- Deductibles, copayments, coinsurance, benefit maximums, waiting periods, or other limitations on coverage for infertility shall not differ from covered services that are unrelated to infertility.
Employers that are exempt from state law
Self-insured employers, religious employers.
Read the Colorado IVF State Laws
C.R.S. 10-16-104
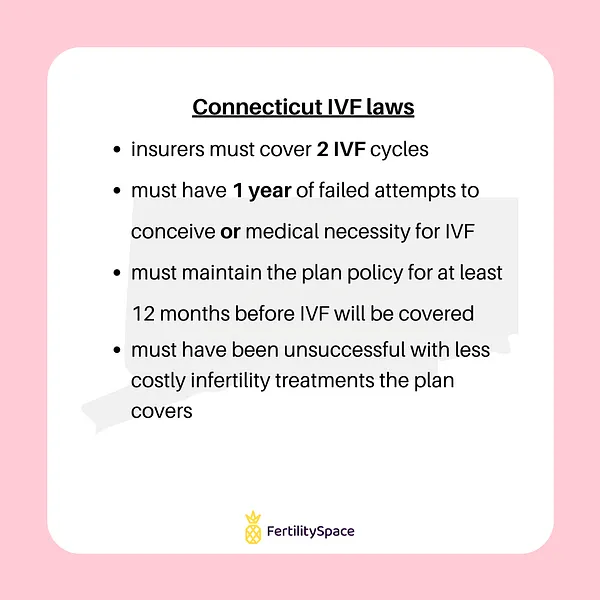
Connecticut
Requirements for IVF coverage
- inability to conceive or sustain a successful pregnancy during a 1 year period or needs treatment due to medical necessity
- must have maintained medical plan policy for at least 12 months
- must have been unable to conceive or sustain a successful pregnancy through less expensive and medically viable infertility treatment
- clinic used must conform to standards of ASRM or SREI
Coverage for infertility treatment in Connecticut includes
- 4 cycles of ovulation induction
- 3 cycles of IUI
- 2 IVF cycles with no more than two embryo implantations per cycle (each fertilization or transfer counts as one cycle)
- male infertility treatment
Egg/sperm freezing coverage
- Harvesting of eggs and sperm is a covered benefit in cases where patients will undergo treatment that has the potential to render them infertile including, but not limited to treatment for cancer.
- Egg/sperm storage is not covered.
Insurance carrier limitations on coverage
- Carriers may apply deductible, coinsurance, copayments to infertility coverage.
- Coinsurance must be within the allowable range of 0% - 50% for the member.
- Carriers cannot set specific limits on infertility treatment other than those specified by the state statutes.
- Coverage does not apply to donor costs, reversal of sterilization, gestational carrier/surrogate parenting arrangements.
Employers that are exempt from state law
Self-insured employers, religious employers.
Read the Connecticut IVF State Laws
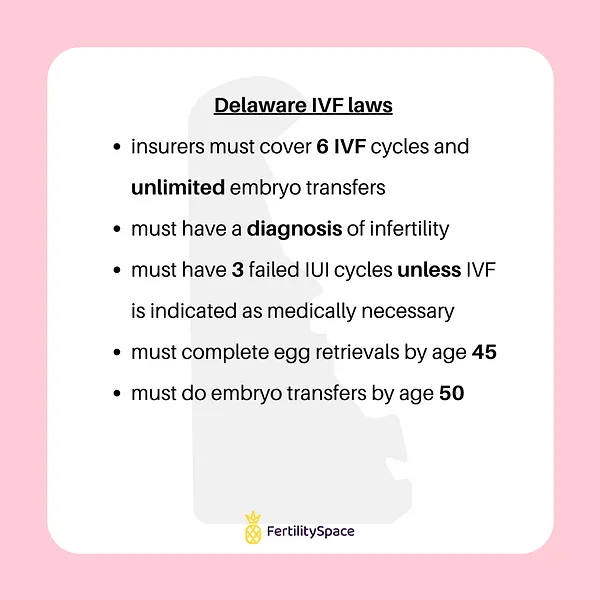
Delaware
Requirements for IVF coverage
- diagnosis of infertility or risk of iatrogenic infertility
- inability to obtain a successful pregnancy through reasonable effort with less costly infertility treatments covered by the policy
- no more than 3 treatment cycles of ovulation induction or IUIs may be required before in vitro fertilization services are covered
- if IVF is medically necessary, no cycles of ovulation induction or IUIs may be required before in vitro fertilization services are covered
- IVF procedures must be performed at a practice that conforms to ASRM and ACOG guidelines
- IVF retrievals are completed before the individual is 45 years old and embryo transfers are completed before the individual is 50 years old
Coverage for IVF in Delaware includes
- intrauterine insemination
- assisted hatching
- cryopreservation and thawing of eggs, sperm, and embryos
- cryopreservation of ovarian tissue
- cryopreservation of testicular tissue
- embryo biopsy
- consultation and diagnostic testing
- fresh and frozen embryo transfers
- 6 completed egg retrievals per lifetime with unlimited embryo transfers, using single embryo transfer (SET) when recommended and medically appropriate
- in vitro fertilization (IVF), including ivf using donor eggs, sperm, or embryos, and ivf where the embryo is transferred to a gestational carrier or surrogate
- intracytoplasmic sperm injection (ICSI)
- medications
- ovulation induction
- storage of oocytes, sperm, embryos, and tissue
- surgery, including microsurgical sperm aspiration
- medical and laboratory services that reduce excess embryo creation through egg cryopreservation and thawing in accordance with an individual’s religious or ethical beliefs
Egg/sperm freezing coverage
Covered for patients who must undergo medically necessary procedures that may cause an impairment of fertility due to surgery, radiation, chemotherapy, or other medical treatment.
Insurance carrier limitations on coverage
- Infertility coverage must be provided to the same extent as other pregnancy-related benefits offered.
- Insurers may not impose any exclusions, limitations, or other restrictions on coverage of fertility medications that are different from those imposed on any other prescription medications.
- Deductibles, copayments, coinsurance, benefit maximums, waiting periods, or any other limitations on coverage fertility may not differ those imposed upon benefits for services unrelated to infertility.
- Insurers are not required to cover experimental fertility services, monetary payments to gestational carriers or surrogates, or the reversal of voluntary sterilization undergone after the covered individual successfully procreated with the covered individual’s partner at the time the reversal is desired.
Employers that are exempt from state law
Religious employers, self-insured employers, and employers with fewer than 50 employees.
Read the Delaware IVF State Laws
Title 18 Subchapter 1, § 3342 and Section 2, § 3556
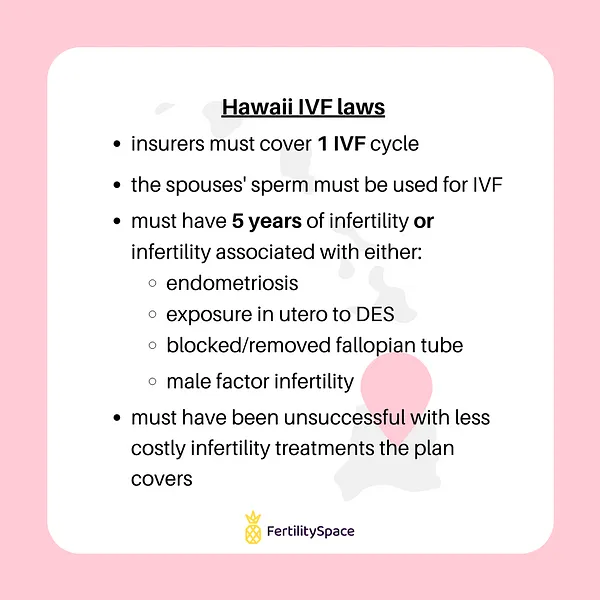
Hawaii
Requirements for IVF coverage
- the patient must be the subscriber or a covered dependent of the subscriber
- oocytes must fertilized with the patient’s spouse’s sperm
- has a history of infertility of at least 5 years duration or
- has infertility associated with one or more of the following medical conditions:
- endometriosis
- exposure in utero to diethylstilbestrol (DES)
- blockage/removal of one or more fallopian tubes
- abnormal male factors contributing to the infertility
- has been unable to attain a successful pregnancy through other applicable infertility treatments for which coverage is available under the contract
- IVF must be performed at a facility that conforms to the guidelines set by ACOG or ASRM
Coverage for IVF in Hawaii includes
One-time only benefit for in vitro fertilization.
Egg/sperm freezing coverage
None specified.
Insurance carrier limitations on coverage
Benefits are provided to the same extent as the pregnancy-related benefits that are covered.
Employers that are exempt from state law
Self-insured employers.
Read your state laws
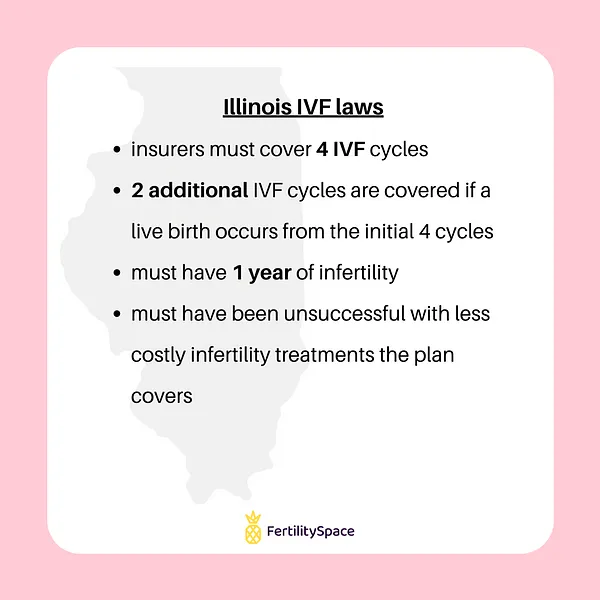
Illinois
Illinois IVF Coverage Limit: 4 IVF cycles. If a live birth follows, then 2 additional IVF cycles are covered.
Chicago Fertility Clinics
Requirements for IVF coverage
- infertility due to either:
- inability to conceive after 1 year of unprotected sexual intercourse
- inability to conceive after 1 year of attempts to produce conception
- inability to conceive after an individual is diagnosed with a condition affecting fertility
- inability to sustain a successful pregnancy
- unable to attain or sustain a successful pregnancy through reasonable, less costly medically appropriate infertility treatments covered under the plan
- must have not exceeded the 4 + 2 oocyte retrieval coverage limit
- medical facility used must adhere to guidelines set by ACOG or ASRM
Coverage for IVF in Illinois includes
- 4 completed oocyte retrievals
- if a live birth results following a completed retrieval, 2 additional oocyte retrievals are covered
- in vitro fertilization
- uterine embryo lavage
- embryo transfer
- artificial insemination
- gamete intrafallopian tube transfer
- zygote intrafallopian tube transfer
- low tubal ovum transfer
Egg/sperm freezing coverage
Covered when a necessary medical treatment may directly or indirectly cause an impairment of fertility by surgery, radiation, chemotherapy, or other medical treatment affecting reproductive organs or processes.
Insurance carrier limitations on coverage
- Insurers that provide pregnancy-related benefits shall also include coverage for infertility.
- For fertility preservation coverage, an insurer shall not discriminate based on an individual's expected length of life, present or predicted disability, degree of medical dependency, quality of life, or other health conditions, nor based on personal characteristics, including age, sex, sexual orientation, or marital status.
Employers that are exempt from state law
Religious employers, self-insured employers, and employers with less than 25 employees.
Read the Illinois IVF State Laws
IL Stat. Section 215 ILCS 5/356m
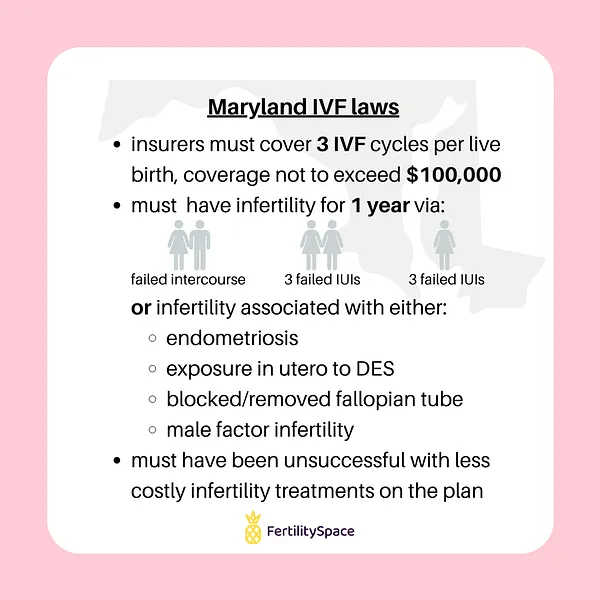
Maryland
Maryland IVF Coverage Limit: 3 IVF cycles per live birth with a total lifetime maximum of $100,000.
Baltimore Fertility Clinics
Requirements for IVF coverage
Married patients:
- opposite-sex couples that have failed to achieve a pregnancy through intercourse for 1 year’s duration
- the patient’s oocytes are fertilized by the patient’s spouse’s sperm, unless:
- the patient's spouse is unable to produce and deliver functional sperm and
- is not a result of a vasectomy/voluntary sterilization
- same-sex couples that fail to achieve a pregnancy after 3 attempts of artificial insemination over the course of 1 year
Unmarried patients:
- the patient has failed to achieve a pregnancy after 3 attempts of artificial insemination over the course of 1 year
Infertility of the patient or patient’s spouse is associated with a condition of:
- endometriosis
- exposure in utero to diethylstilbestrol (DES)
- blockage/removal of one/both fallopian tubes
- abnormal male factors such as oligospermia contributing to infertility
IVF will be covered if patients have been unable to achieve a successful pregnancy through a less costly infertility treatment covered under the plan.
IVF must be performed at a medical facility that adheres to guidelines and minimum standards of ACOG or ASRM.
Coverage for IVF in Maryland includes
- 3 IVF cycles
- $100,000 lifetime maximum for infertility coverage
Egg/sperm freezing coverage
- Egg/sperm freezing is covered for an enrollee that needs medical treatment which may directly or indirectly cause infertility by surgery, chemotherapy, radiation or other medical treatment affecting the reproductive organs or processes.
- Egg/sperm storage is not covered.
Insurance carrier limitations on coverage
Donor sperm obtainment not covered under insurance.
Employers that are exempt from state law
Religious employers, self-insured employers, and small employers.
Read the Maryland IVF State Laws
MD Insurance Code Ann. Section 15-810
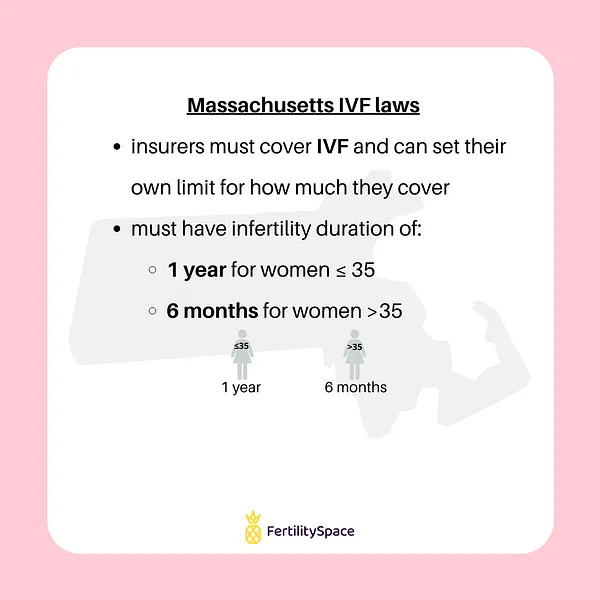
Massachusetts
Massachusetts IVF Coverage Limit: No lifetime limit set by the state, insurers may set a maximum coverage limit.
Boston Fertility Clinics
Requirements for IVF coverage
- inability to conceive for 1 year is the female patient is aged 35 or younger
- inability to conceive for 6 months if they female patient is over the age of 35
If the individual conceives but is unable to achieve a live birth in the pregnancy, this period of time the patient attempted to conceive prior to pregnancy will be included in the calculation of the 1-year/6-month period for infertility.
Coverage for infertility treatments in Massachusetts includes
- artificial insemination (AI) and intrauterine insemination (IUI)
- in vitro fertilization and embryo transfer (IVF-ET)
- gamete intrafallopian transfer (GIFT)
- sperm, egg and/or inseminated egg procurement and processing, and banking of sperm or inseminated eggs, to the extent such costs are not covered by the donor's insurer, if any
- intracytoplasmic sperm injection (ICSI) for the treatment of male factor infertility
- zygote intrafallopian transfer (ZIFT)
- assisted hatching
- cryopreservation of eggs
Egg/sperm freezing coverage
None listed.
Insurance carrier limitations on coverage
- Limitations/restriction on coverage for infertility-related drugs shall not differ from those imposed on other prescription drugs.
- Deductibles, coinsurance, copayments or benefit maximums for infertility shall not differ from benefits that are unrelated to infertility.
- Insurers will not impose exclusions based on pre-existing conditions or impose a pre-existing condition waiting period on infertility coverage.
- Insurers are not required to provide coverage for experimental procedures, surrogacy, or reversal of voluntary sterilization.
Employers that are exempt from state law
Self-insured employers.
Read the Massachusetts IVF state laws
Mass Gen Laws Ann. Ch. 175, Section 47H, ch. 176A, Section 8K, ch.176B, Section 4J, ch 176G, Section 4, and 211 CMR 37.00
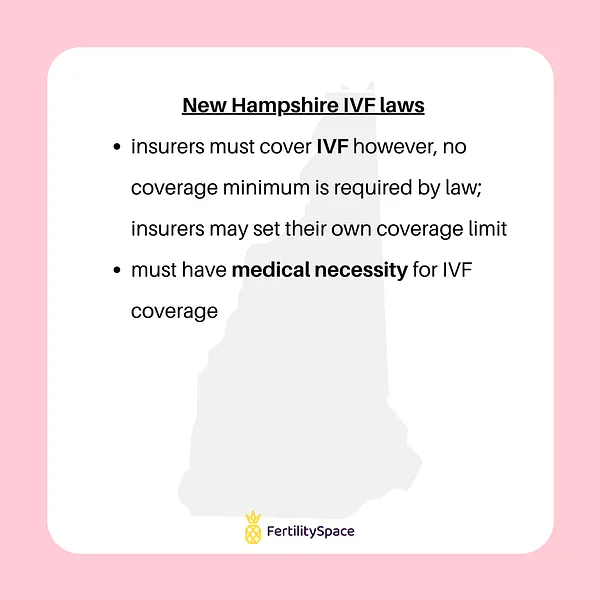
New Hampshire
New Hampshire IVF Coverage Limit: No coverage limit set by the state, max coverage may depend on your specific insurance plan.
Fertility Clinics Near Manchester, New Hampshire
Requirements for IVF coverage
Coverage for infertility treatment due to medical necessity.
Coverage for IVF in New Hampshire includes
- evaluations
- laboratory assessments
- medications
- treatments associated with the procurement of donor eggs, sperm, and embryos
Egg/sperm freezing coverage
- Covered for a policy holder that is expected to undergo surgery, radiation, chemotherapy, or other medical treatment that is recognized by medical professionals to cause a risk of impairment of fertility.
- Storage is covered from the time of cryopreservation for the duration of the policy term.
- Storage for a longer period of time may be offered by the insurer as an optional benefit.
Insurance carrier limitations on coverage
- Deductibles, copayments, coinsurance or benefit maximums, waiting periods or other limitations on coverage shall not differ from benefits that are unrelated to infertility.
- Limitations of infertility medication coverage shall not differ from limitations imposed on other prescription medications.
- Limitations on coverage shall not be based solely on arbitrary factors including, but not limited to, number of attempts or dollar amounts or age.
- Insurers shall not provide different benefits to, or impose different requirements upon, a class protected under RSA 354-A than that provided to, or required of, other patients.
- Insurers will not cover experimental infertility procedures, non-medical costs related to third party reproduction, or reversal of voluntary sterilization.
- An enrollee's coverage shall not extend to medical costs relating to the preparation for reception or introduction of embryos, oocytes, or donor sperm into a surrogate or gestational carrier when utilizing a surrogate or gestational carrier due to a medical cause of infertility unrelated to voluntary sterilization or failed reversal.
Employers that are exempt from state law
Employers that utilize the Small Business Health Options Program (SHOP) or Extended Transition to Affordable Care Act-Compliant Policies.
Read the New Hampshire IVF State Laws
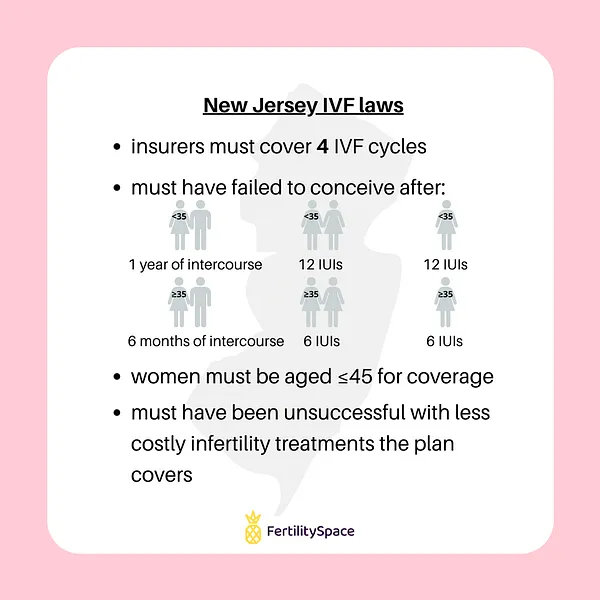
New Jersey
Requirements for IVF coverage
- infertility defined by either:
- a male who is unable to impregnate a female
- a female with a male partner and under 35 years of age is unable to conceive after 12 months of unprotected sexual intercourse
- a female with a male partner and 35 years of age and over is unable to conceive after six months of unprotected sexual intercourse
- a female without a male partner and under 35 years of age who is unable to conceive after 12 failed attempts of intrauterine insemination under medical supervision
- a female without a male partner and over 35 years of age who is unable to conceive after six failed attempts of intrauterine insemination under medical supervision
- partners are unable to conceive as a result of involuntary medical sterility
- a person is unable to carry a pregnancy to live birth or
- a previous determination of infertility pursuant to this section
- has used all reasonable and less expensive treatment prior to IVF and is still unable to achieve or carry a successful pregnancy
- is 45 years of age or younger for IVF coverage to apply
- receives infertility services from a medical facility that conforms to the guidelines of ACOG or ASRM
Coverage for IVF in New Jersey includes
- diagnosis and diagnostic tests
- medications
- surgery
- artificial insemination
- gamete intra fallopian transfer (GIFT)
- zygote intra fallopian transfer (ZIFT)
- intracytoplasmic sperm injection (ICSI)
- in vitro fertilization (IVF)
- embryo transfer
- 4 completed egg retrievals per lifetime of the covered person
Egg/sperm freezing coverage
- Egg or sperm freezing is covered due to an impairment of fertility caused by surgery, radiation, chemotherapy, or other medical treatment affecting reproductive organs or processes.
- Oocyte or sperm storage costs are not covered.
Insurance carrier limitations on coverage
- Copayments, deductibles and benefit limits for infertility will be the same as those applied to other medical or surgical benefits under the contract.
- Coverage will not be determined based on a covered person's expected length of life, present or predicted disability, degree of medical dependency, perceived quality of life, or other health conditions, or based on personal characteristics, including age, sex, sexual orientation, marital status, or gender identity.
- Coverage will not apply for infertility due to voluntary sterilization.
Employers that are exempt from state law
Self-insured employers, religious employers, and employers with fewer than 50 employees.
Read the New Jersey IVF State Laws
New Jersey revised Statutes Chapter 236, 52:14-17029v, 52:14-17.46.6g, Section 52:14-17.29bb, 52:14-17.46.6m
On NJgov site, you’ll need to type in the applicable section into the search bar so that you can read it.
New York
Requirements for IVF coverage
infertility defined by either:
- failure to establish a clinical pregnancy after 12 months of regular, unprotected sexual intercourse or therapeutic donor insemination
- failure to establish a clinical pregnancy after 6 months of regular, unprotected sexual intercourse or therapeutic donor insemination for a female aged 35 or older
- earlier evaluation and treatment may be warranted based on an individual's medical history or physical findings
Coverage for IVF in New York includes
- hysterosalpingogram
- hysteroscopy
- endometrial biopsy
- laparoscopy
- sonohysterogram
- post-coital tests
- testis biopsy
- semen analysis
- blood tests
- ultrasound
- prescription fertility drugs (approved by the FDA)
- 3 IVF cycles (fresh transfer or a frozen embryo transfer)
Egg/sperm freezing coverage
Covered when a medical treatment may directly or indirectly cause an impairment of fertility by surgery, radiation, chemotherapy or other medical treatment affecting reproductive organs or processes.
Insurance carrier limitations on coverage:
- Co-payments, coinsurance and deductibles for infertility coverage are to be consistent with those established for other benefits within a given policy.
- Insurers will not discriminate coverage based on an insured's expected length of life, present or predicted disability, degree of medical dependency, perceived quality of life, or other health conditions, nor based on personal characteristics, including age, sex, sexual orientation, marital status or gender identity.
- Coverage will not apply to experimental treatments and procedures based on the standards and guidelines of ACOG and ASRM.
Employers that are exempt from state law
Self-insured employers, individual & small group policies.
Read the New York IVF State Laws
NY Insurance Law Section 3216 (13), Section 3221, Section 4303, Section 3216 (13) (C), FY 2020 NYS Budget
As of February 15, 2021, New York State has legalized compensated gestational surrogacy.
As of February 15, 2021, New York State has legalized compensated gestational surrogacy.
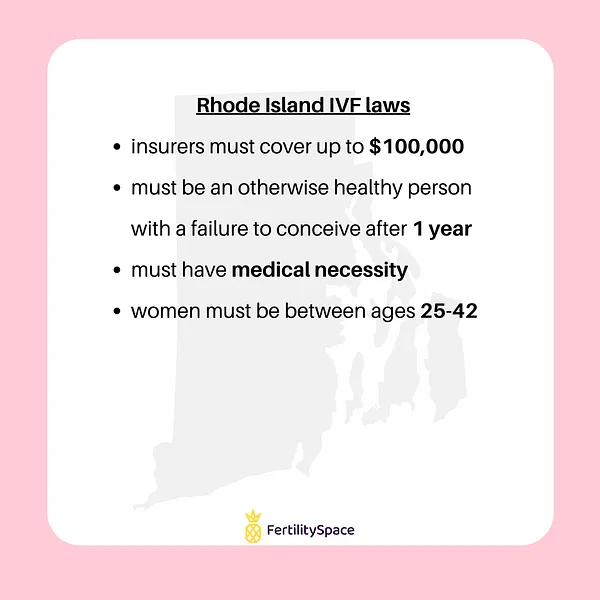
Rhode Island
Requirements for IVF coverage
- an otherwise healthy individual who is unable to conceive or sustain a pregnancy over a duration of 1 year
- must have medical necessity for diagnosis and treatment of infertility
- women must be between the ages of 25 and 42
Coverage for IVF in Rhode Island includes
Specific testing and treatment procedures are not listed.
Egg/sperm freezing coverage
Covered when medically necessary medical treatment may directly or indirectly cause an impairment of fertility by surgery, radiation, chemotherapy, or other medical treatment affecting reproductive organs or processes.
Insurance carrier limitations on coverage
- Policies that include pregnancy-related benefits will also provide infertility coverage.
- Carriers may impose a lifetime maximum of $100,000 for infertility coverage.
- Enrollee co-payment shall not exceed 20% for infertility services.
Employers that are exempt from state law
Self-insured employers & health insurance contracts providing supplemental coverage to Medicare or other governmental programs.
Read the Rhode Island IVF State Laws
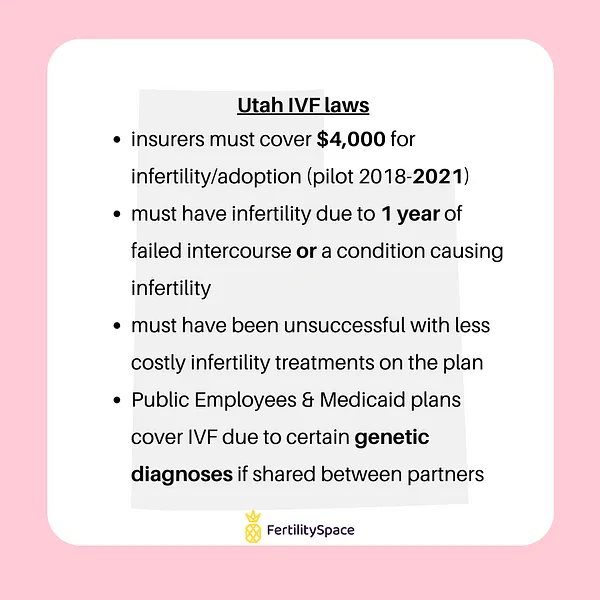
Utah
Utah IVF Coverage Limit: $4,000 lifetime maximum (Pilot program in effect 2018-2021)
Salt Lake City Fertility Clinics
Requirements for IVF coverage
Pilot program (2018-2021)
- the insured has coverage for maternity benefits under the plan
- infertility is demonstrated by either:
- physician verification that the patient or the patient's spouse has a demonstrated condition recognized by a physician as a cause of infertility
- the patient attestation the inability to conceive or carry a pregnancy to a live birth after 1 year or more of regular sexual relations without contraception
- the patient attests to the inability to attain a successful pregnancy through any less-costly, potentially effective infertility treatments covered under the health plan
- procedures are performed at a medical facility that conforms to the minimal standards set by ASRM
Public Employees benefits & Medicaid enrollees will have IVF coverage if:
- a covered individual has been diagnosed by a physician as having a genetic trait associated with a condition of either:
- cystic fibrosis
- spinal muscular atrophy
- Morquio syndrome
- myotonic dystrophy
- sickle cell anemia
- the individual intends to get pregnant with a partner who is diagnosed by a physician as having a genetic trait associated with the same qualified condition as the covered individual
Coverage for IVF in Utah includes
Pilot program (2018-2021)
- $4,000 lifetime maximum coverage of each qualified individual
- benefit may be used for infertility treatment coverage or as an indemnity benefit for adoption
Public Employees benefits & Medicaid enrollees
- in vitro fertilization (IVF)
- genetic testing
Egg/sperm freezing coverage
None listed.
Insurance carrier limitations on coverage
Pilot program (2018-2021)
- Insurers must provide written disclosure to a potential enrollee whether the insurer will permit an exchange of the adoption indemnity benefit for infertility treatment instead.
- Coverage for infertility will apply to the same cost-share as the medical plan.
Pilot program notes
- The purpose of the pilot program is to study the efficacy of providing coverage for the use of an assisted reproductive technology and is not a mandate for coverage of an assisted reproductive technology within all health plans offered by the program.
- Before November 30, 2021, the program shall report to the Social Services Appropriations Subcommittee regarding the costs and benefits of the pilot program.
Employers that are exempt from state law
Self-insured employers.
Read the Utah IVF State Laws
🕵️♀️ Ready to schedule with a fertility clinic? Find fertility doctors near you. See their IVF success rates and read past patient reviews!